Tests and Investigations: Bloods and Gastroscopy
So far to date these are the investigations I have had:
Blood work
I have had lots of blood work done to rule out potential postnatal problems that may cause nausea and vomiting such as postpartum thyroiditis which can affect up to 5% of women after the birth of their babies. This can give symptoms of nausea and vomiting. This is more likely if you have a pre-existing thyroid condition. As I had already suffered with Hypothyroidism since 2007, I was at a greater risk of having this. My blood work was also to rule out any other imbalances, conditions or infections I may have got after delivering my baby. My blood work showed I had an increased calcium level and that I was deficient in a few vitamins and minerals. To this day it was unknown what caused my elevated calcium level. It was back to a normal range at the next blood test. However electrolyte and vitamin deficiencies are very common in patients with prolonged nausea and vomiting. I was prescribed replacements to correct the imbalances and monitored.
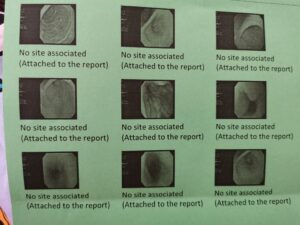
Gastroscopy
In February 2021. I had a gastroscopy, this is a outpatient procedure where doctors will look in the stomach with an endoscope to look for any obstructions or abnormalities that could explain what would cause the nausea and vomiting. An obvious cause would be if there was a blockage or physical problem within the stomach such as an ulcer. I chose to be sedated for this procedure after having a very traumatic NJ tube endoscopic surgery which I still get flashbacks to this day from.
During this procedure I was instructed that I was not allowed to eat 8 hours before and not allowed to drink 3 hours prior the the procedure. After arriving at the endoscopy unit, I had my vital signs like temperature, blood pressure checked. I had a cannula inserted into the back of my hand and then taken through to the theatre. I had some local anaesthetic sprayed to the back of my throat. This was fairly unpleasant. And then had a plastic mouth guard put in my mouth to hold my mouth open. I was then given the sedative (Midazolam) through my cannula. I do not remember anything more, as this made me completely sleepy. It is not like a full anaesthetic where you are completely under but sleepy enough that you cannot remember the procedure. Some people chose to stay conscious for this, making the recovery a lot quicker. Having the sedation means you need a responsible adult with you for 24 hours after and cannot be in charge of children etc.
I had some local anaesthetic sprayed to the back of my throat. This was fairly unpleasant. And then had a plastic mouth guard put in my mouth to hold my mouth open. I was then given the sedative (Midazolam) through my cannula. I do not remember anything more, as this made me completely sleepy. It is not like a full anaesthetic where you are completely under but sleepy enough that you cannot remember the procedure. Some people chose to stay conscious for this, making the recovery a lot quicker. Having the sedation means you need a responsible adult with you for 24 hours after and cannot be in charge of children etc.
During the gastroscopy whether you are sedated or conscious the endoscope is put in your mouth and down your throat and will look at your digestive tract and in your stomach for signs of abnormalities. The doctors will take picture and biopsies which can be later seen under a microscope to look for conditions like crohns disease and cancer. I had 6 biopsies taken, which came back as normal.
Despite having had nothing to eat for over 13 hours the doctors discovered food still in my stomach which was signs that I had delayed gastric emptying. This could be a sign of a motility problem such as gastroparesis which would cause the symptoms I had been having. The doctors also noted that I had some atrophy to the antrum part of my stomach. This could be a sign of a condition called Gastritis but also a sign of my prolonged vomiting.
Photos taken during my gastroscopy
After the procedure I was wheeled to recovery and once awake, my vital signs were monitors for 30 minutes. Once fully awake, my cannula was removed and I was allowed to leave once someone came to collect me. I made a quick recovery but was a bit tired for the rest of the day. The sedation is quick acting but can make you very sleepy for the next 24 hours.
For me the most difficult part of this was procedure was being back in the same endoscopy unit, at the same hospital I had my NJ tube put in. I had a very traumatic time where I awoke from an endoscopic surgery to stitch a feeding tube into my jejunum and it brought back a lot of bad memories of pain and being held down. It was quite hard to face but I had to get on with it as this was an important step into diagnosing my current problem. After having a bit of a cry and a chat with the nurses, who were fantastic and very reassuring I was able to get the courage to go ahead with the gastroscopy. The procedure itself went well, I had no pain and don’t remember anything. But it is worth saying that there are a few small risks when you have this done. You can get a bit of a sore throat, and there are small chances of injury or bleeding from the scope, however this is rare. I had no after effects.
Because of the results, it was decided the the delayed gastric emptying needed further looking in to and so my consultant then referred me on for investigations into how my stomach was digesting food. I was put on the waiting list for a gastric emptying study.
My Gastroscopy Report
For more information about Gastroscopies please visit:
https://www.nhs.uk/conditions/gastroscopy/what-happens/