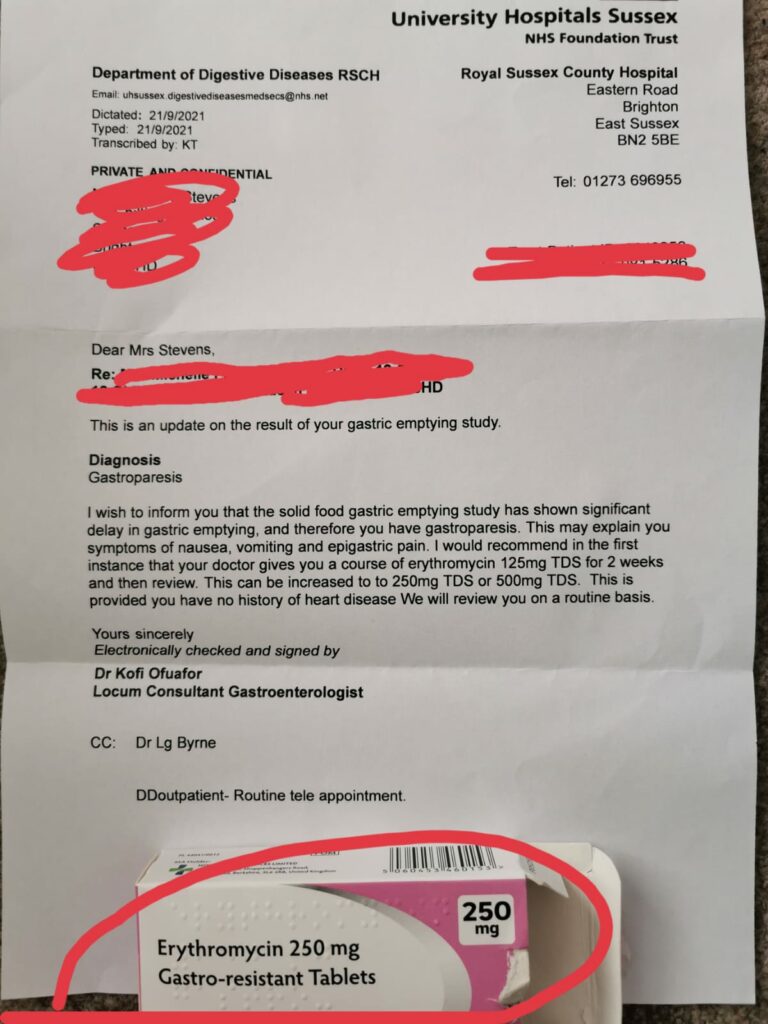
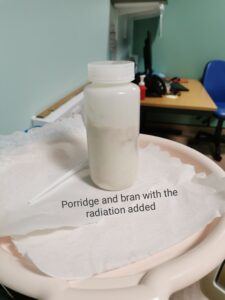
So weeks after these were due I finally have the result of my gastric emptying scan and to be honest I was pretty shocked by them! I thought I had a motility problem but I just didn’t realise how bad it was.
It seems that during the time I was at the hospital for the gastric emptying scan the food barely moved at all, there was only a tiny amount that was digested that they couldn’t measure it precisely. With the pictures and data they collected Doctors could see that it would take my stomach 910 minutes to half empty. 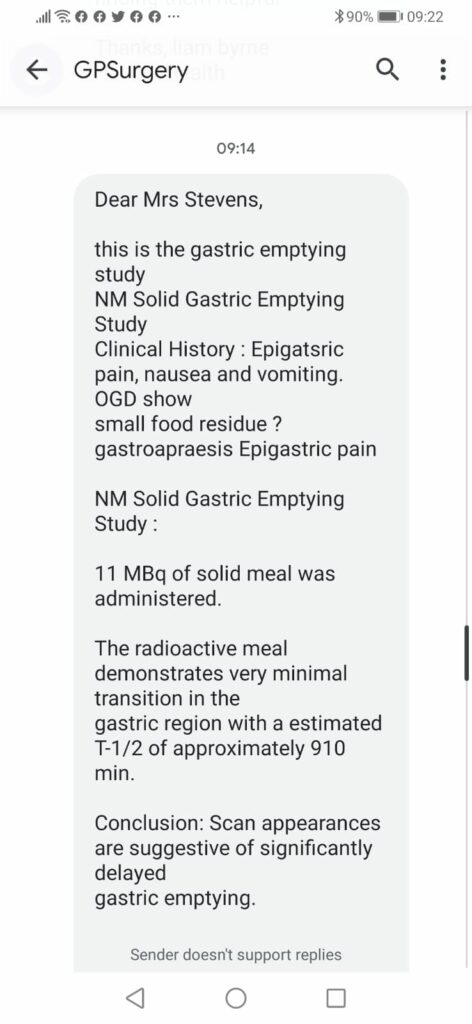 The average person takes between 43-115 minutes to half empty so my stomach was significantly slower than it should be. My GP had the results before the consultant and diagnosed me with severe gastroparesis, with this result, my symptoms and my continued weight loss he has suggested a feeding tube. My dietician also suggested this and asked for me to be referred to endoscopy for a feeding tube placement.
The average person takes between 43-115 minutes to half empty so my stomach was significantly slower than it should be. My GP had the results before the consultant and diagnosed me with severe gastroparesis, with this result, my symptoms and my continued weight loss he has suggested a feeding tube. My dietician also suggested this and asked for me to be referred to endoscopy for a feeding tube placement.
I don’t know how I feel about ‘needing’ a tube, I feel upset with myself and my stomach for not working properly and i’m frightened about having to rely on a tube again and not eat normally. However it has been a long time since I have been able to eat properly anyway. I have to avoid eating in public or going out for meals with friends and family because I can end up vomiting so I often avoid it or take double of my medication. If I take double medication, It can stop me vomiting (until the meds wear out) but it doesn’t stop me getting the same excruciating pain I usually get. It is so much easier to vomit sooner and end the pain quicker than delay the vomiting and have to deal with the agony until my the medication wears off and I end up vomiting hours later. So eating ‘normally’ has already been something that I cannot do.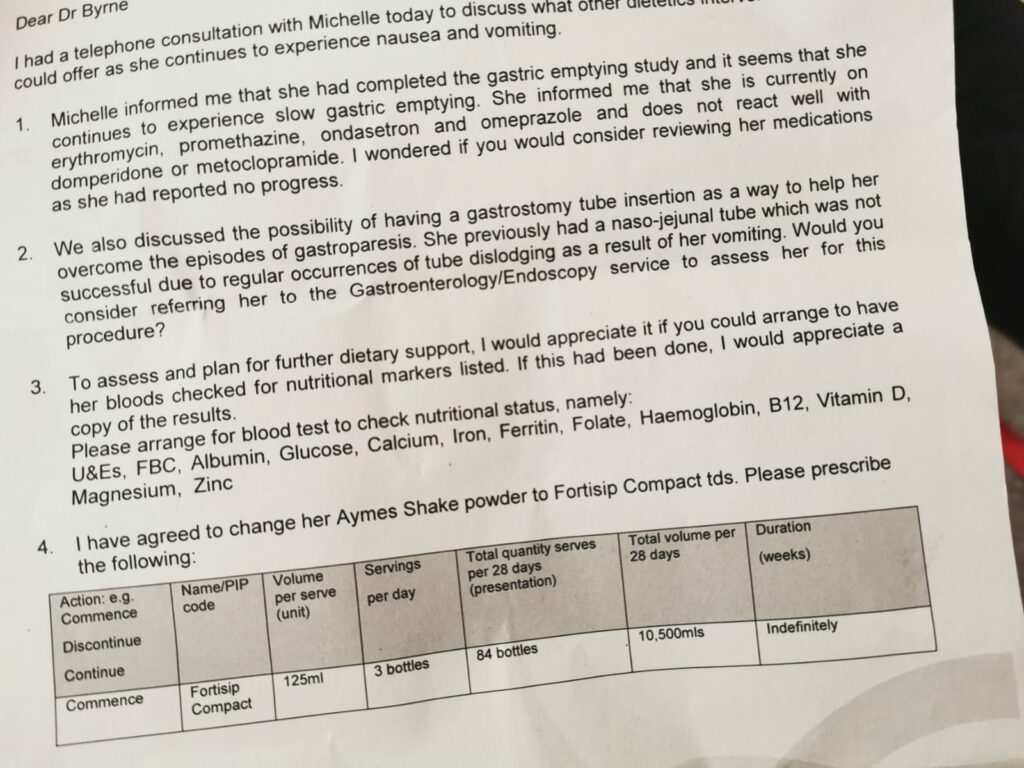
I worry about the procedure of the tube itself. My dietician is thinking they will give me a gastronomy or gastro-jejunal tube (G-tube or GJ tube), which is surgically placed and comes with quite a long recovery. I worry about how I will cope with the pain of it, especially with a little toddler running around.
On the other hand I really welcome having some nourishment back, being able to feel like I have more energy. Not getting enough nutrients is affecting my body in lots of different ways: My periods have not come back since the birth, early onset menopause, thin and dry hair that breaks easily. My nails are brittle and break easily. I am ALWAYS so tired and cold, I have to wear 3 layers of clothes inside and 2 pairs of socks, even with the heating turned on. My hips hurt when I sit on a hard chair/bench or in the bath. Laying in bed is uncomfortable where I have so little fat. I am so irritable and my mood is so up and down. I am prescribed medication for my mental health condition but it doesn’t always stay down so my mental health in uncontrolled. I hate how I look now, I don’t look healthy and always have such heavy eye bags. Having the tube giving me some nutrients can improve all of this for me and give me such a better quality of life, so I welcome the idea of this.
In the last few weeks my weight has continued to drop and I hit a new low of 115lbs, my GP has asked that I get an expedited urgent appointment for this tube, so now I am waiting for an urgent appointment with my gastroenterologist to discuss the need for the tube. In the meantime he has doubled my erythromycin medication. Unfortunately I don’t find this medication helps me at all and i’m allergic to metoclopramide and domperidone! However due to the delay in appointments because of the pandemic I have been warned that even urgent appointments are taking a long time. I just hope its soon because I am really struggling now, this condition is getting me down! For nutrition I have Fortisip milkshake supplements that contain minerals and are full of calories but I often struggle to keep these down as they are quite heavy on my stomach.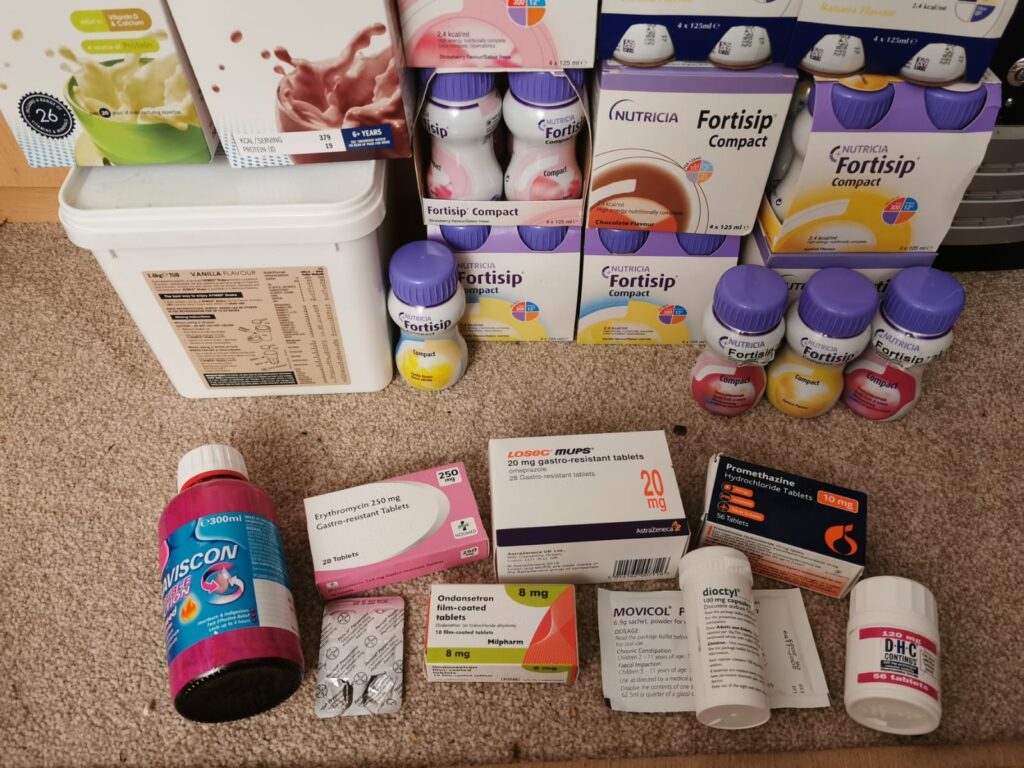






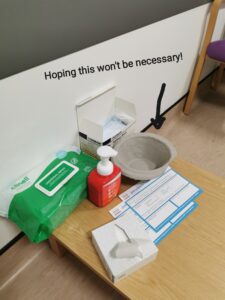
 I had some local anaesthetic sprayed to the back of my throat. This was fairly unpleasant. And then had a plastic mouth guard put in my mouth to hold my mouth open. I was then given the sedative (Midazolam) through my cannula. I do not remember anything more, as this made me completely sleepy. It is not like a full anaesthetic where you are completely under but sleepy enough that you cannot remember the procedure. Some people chose to stay conscious for this, making the recovery a lot quicker. Having the sedation means you need a responsible adult with you for 24 hours after and cannot be in charge of children etc.
I had some local anaesthetic sprayed to the back of my throat. This was fairly unpleasant. And then had a plastic mouth guard put in my mouth to hold my mouth open. I was then given the sedative (Midazolam) through my cannula. I do not remember anything more, as this made me completely sleepy. It is not like a full anaesthetic where you are completely under but sleepy enough that you cannot remember the procedure. Some people chose to stay conscious for this, making the recovery a lot quicker. Having the sedation means you need a responsible adult with you for 24 hours after and cannot be in charge of children etc.